What is Colitis – the cause of mucoid gooey stool?
Colitis means that the colon or large intestine is inflamed. The hallmark of colitis is a gooey, frequent diarrhea that may contain blood and/or mucus.

The stool may start normal then finish soft or may seem gooey throughout. There is often accompanying gas and the sudden need to run for a bathroom.
Vomiting can go along with colitis but the primary feature is the gooey diarrhea. Colitis may happen suddenly or can be going on for a while. Weight loss is often not a common feature.
A Little About the Colon

the colon/lower intestine is the last segment of the digestive tract. Before reaching the colon, food has been digested and mostly absorbed. What’s left is the waste products from food, the feces, and this is eliminated by the colon.
The colon has three functions:
- Absorbing water
- storing stool
- Digesting unabsorbed nutrients
The bacterial population in the colon is about 10 times more dense than that of the small intestine. These bacteria, often referred to as good or helpful bacteria, take fibers that were undigestible to the host and actually process them into biochemicals that provide nourishment to the colon cells.
The bacteria that live in the colon not only feed the cells of the colon, but they also control the pH of the colon environment so that excreted toxins are trapped in the stool and will be pooped away rather than be reabsorbed back into the body.
Diarrhea Can Come from Either the Small Intestine or the Large Intestine and the Approach is Different in Either Case
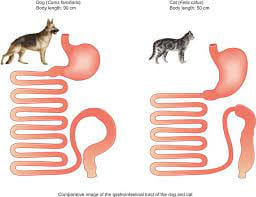
In classifying diarrhea, it is important to determine whether the problem originates from the small intestine, the colon, or possibly both. Small intestinal diarrheas tend to be more serious as it involves problems digesting and absorbing nutrients from food.
Diarrhea of the colon is less debilitating but still uncomfortable. The following are characteristics of large intestinal diarrhea:
- Large intestinal diarrheas are generally not associated with weight loss and patients generally have normal energy levels and normal appetites.
- Large intestinal diarrhea is associated with straining to defecate. Often this straining is unproductive, leading to the erroneous conclusion that the patient is constipated.
- There is cramping, flatulence, and a sudden sense of urgency. The pet may not be able to get to an appropriate area before the diarrhea erupts.
- Mucus or slime may be seen in the stool along with often fresh blood
- The stool may begin looking normal and formed but finish as a puddle.
A diagnosis of colitis is generally straight forward given the above classic findings, though how to proceed depends on the signs. Is the problem acute (i.e., suddenly there) or chronic (has been happening for several weeks regularly) or episodic (happens then goes away then happens again)?
Colitis Suddenly
A pet that has sudden symptoms of colitis probably has a stress-related colitis (common after boarding, moving, severe weather or other change) or a dietary indiscretion-related colitis (usually involves treats or raiding the garbage).
These episodes should be treated immediately as they can get worse if left untreated. That said, in general, colitis can be treated with a short course of medication such as metronidazole, probiotics and dietary therapy.

Parasites, especially Giardia and whipworms, can also cause colitis and the pet may be tested for those to rule them out or be dewormed. In general, a few days of medication and a bland diet should resolve the problem and the pet will be back to normal quickly.
During recovery, it is common for the pet to have no stool at all for a couple of days. This is normal and not a sign of constipation. If, however, the pet’s diarrhea is not clearly improved in two to three days, contact the veterinarian to see if further testing is needed.
Colitis Chronically or in Recurrent Episodes
If the symptoms of colitis have been going on for a month or more or if they keep recurring and resolving over and over, then a medical work up is needed. It is important to make sure simple causes of colitis have been ruled out, so parasite testing becomes especially important. A good fecal examination for worms and coccidia plus testing additional for giardia should be performed.
If any of these tests are positive, then obviously the parasite in question can be addressed; it is always best to identify the cause of the colitis if it is possible to do so. That said, even if these tests are negative, it is still a good idea to include a broad spectrum de-worming and coccidia treatment should probably be given as these treatments are safe and inexpensive.
Whipworms, in particular, are difficult to detect and commonly cause colitis symptoms. We want to be sure we have ruled out the simple causes of colitis before more advanced diagnostics begin.
Similarly, a week or so of metronidazole may effectively treat a toxin-producing Clostridium perfringens infection and potentially solve the entire problem.
Of course, a basic blood panel and urinalysis are in order, as they are with any chronic disease, to assess the patient’s general health.
If all the regular diagnostics are negative or inconclusive, there is a fecal panel that amplifies DNA of bacterial and protozoal organisms that cause diarrhea. Talk to your veterinarian about this.
Further workup can be initiation of a hypoallergenic diet for food allergies/sensitivities as well as inflammatory bowel disease (IBD). To make a definitive diagnosis of IBD, colonoscopy and intestinal biopsies
Management of Colitis
Colitis is best managed when its cause is known and specific therapy can be instituted. When this is not possible, symptomatic management as described above is often attempted.
Boxers and Some Other Breeds Can Get a Specific Form of Colitis

This condition is also called Boxer colitis because the Boxer breed seems predisposed. This form of colitis is particularly ulcerative and involves infiltration of the tender colon lining with cells called histiocytes.
These cells are the cells that are normally called into the scene of inflammation relatively late so that they can absorb the dead cells and debris that have been created by the inflammatory event.
Dogs with this condition typically show symptoms at an early age (less than two years) and become more debilitated than typical colitis patients. It is currently believed that this condition results from an inappropriate immune response against the common bacteria of the colon, especially E. coli.
Dogs with this form of colitis do not respond well to the usual remedies listed above but instead seem to show an excellent response to one class of antibiotic.
Histiocytic ulcerative colitis can be confirmed by biopsy, although signs of colitis in a young Boxer are highly suggestive of this condition.


