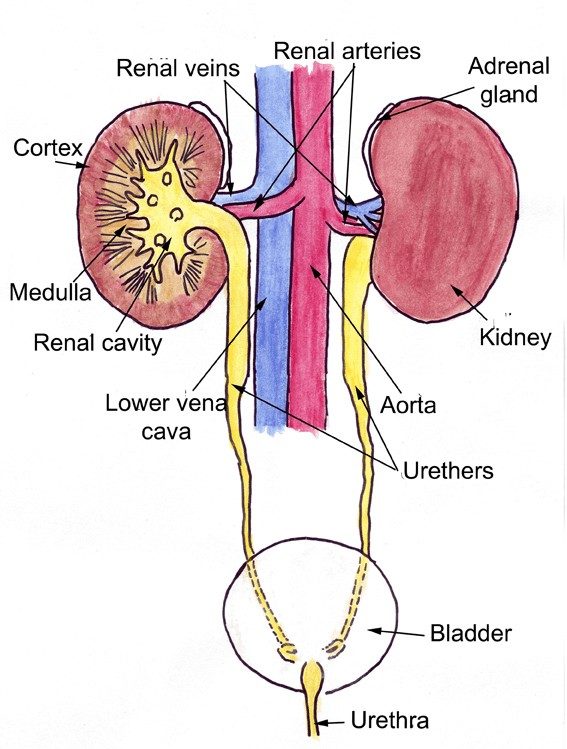
The kidneys do many things to help support the body. One primary role it plays is eliminating toxins that the body metabolizes daily. When the kidneys become begin to lose function, they cannot eliminate toxins from the body and a buildup is created. Additionally, there are other functions that are affected including blood pressure regulation and calcium and phosphorous balance.
Kidney Failure, Chronic Renal Failure, Renal Insufficiency and Insufficient Kidney Function
All of these terms mean the same thing: the kidneys can’t keep up with their daily work. In the past, kidney failure was the predominant term but as these words conjure up images of on-going sickness, expensive hospitalization, and doom they have been largely put aside for terms such as renal insufficiency and insufficient kidney function. After all, loss of kidney function can be mild, moderate, or severe. Recommended treatment is different depending on which jobs the kidneys are not keeping up with and how bad the loss actually is.
Normal kidney function goes far beyond simply making urine. Below lists the tasks performed by normal kidneys:
What Kidneys Do / What Happens When They are Diseased
Water Conservation
Hydration of the body depends not only on water consumed but on water retained by the body, which is done through the kidneys. In times of dehydration, the kidney must respond by conserving water.
Similarly, if you drink too much water, the kidney needs to efficiently remove the excess to prevent dilution of the blood stream. A pet with insufficient kidney function will not be able to make a concentrated urine and will need to drink extra water to process the body’s waste chemicals. For this reason, excessive water consumption is an important early warning sign.
Toxin Removal
When
we analyze a urine sample, one of the most important parameters is the
specific gravity, a measure of how concentrated a urine sample is. Water
has a specific gravity of 1.000. A dilute urine sample has a specific
gravity less than 1.020 (often less than 1.015). A concentrated urine
sample would have a specific gravity over 1.030 or 1.040. A failing
kidney by definition cannot make a concentrated urine and the patient
must drink excessively to get enough water to excrete the day’s toxic
load.
The kidneys remove our metabolic wastes for us. If there is inadequate circulation going through the kidneys or if there are not enough functioning kidney tissue to handle the waste, toxins will build up. If the toxins build up to a level where the patient actually feels sick, a condition called uremia exists. If we can keep our patients below the uremia level, they will feel pretty normal and have good life quality.
There are four markers of kidney failure and toxin buildup:
1) creatinine
2) SDMA (symmetrical dimethylarginine)
3) BUN (blood urea nitrogen).
4) Urine Specific Gravity
These parameters are considered to determine how advanced the renal insufficiency is. It is important to note, however, that dehydration will raise all three of these parameters so the true renal stage will not be evident until the patient is rehydrated.
Calcium/Phosphorus Balance
The
balance between calcium and phosphorus in the blood is important. Too
much of one or the other will lead to crystals forming in the tissues of
the body and weakening of the bones to the extent they may actually
become rubbery. The kidney plays an important role in this balance and
when kidney function is lost, phosphorus levels begin to rise. Therapy
for insufficient kidney function requires monitoring of phosphorus
levels and the use of diet and medications to keep phosphorus levels in a
reasonable range.
Sodium/Potassium Balance
The
kidney plays a major role in controlling electrolyte balance as well.
In particular, conservation of potassium is an important aspect.
Insufficient kidneys lose their ability to conserve potassium and
potassium levels begin to drop leading to weakness. Potassium
supplements are commonly needed in the treatment of kidney failure.
Blood Pressure Regulation
Blood
pressure sensors in the kidney help regulate blood pressure in the
body. When these are damaged, hypertension (high blood pressure) can
result and can damage the kidney further. Blood pressure is commonly
measured in kidney failure patients.
Protein Conservation
There
are a lot of important proteins circulating in the bloodstream and it
is crucial that they are not lost in urine. The nephron possesses a
filtration system that keeps protein in while removing harmful wastes.
If this filtration system is damaged (glomerular disease) then a much
more severe form of kidney failure results. Screening for this damage is
an important aspect of staging kidney failure and a test called a urine
protein:creatinine ratio is often included in the testing profile to
assess this condition.
Red Blood Cell Production
The
kidney produces a hormone called erythropoietin. This hormone tells the
bone marrow to make more red blood cells. In the absence of this
hormone, a non-responsive anemia occurs and can get so bad that
transfusion is necessary. Erythropoietin can be given by injection to
alleviate this problem but there are some potential pitfalls in doing
this. Hematocrit and PCV (packed cell volume) are measures of red blood
cell volume that are commonly monitored in kidney patients.
pH Balance
Metabolic
processes require a narrow pH range for efficiency. The kidney also
regulates this balance and if it cannot, intervention is necessary,
usually in the form of fluid therapy.
Staging and Sub-Staging
The International Renal Interest Society (IRIS) has posed the following staging criteria for pets with Stage I being pets with evidence of kidney disease but no evidence of a change in actual kidney function, all the way up to Stage IV where pets begin to feel sick from their disease. These stages are based on blood creatinine levels measured in mg/dl. It is worth noting that many patients are well past IRIS Stage IV at the time of diagnosis with creatinines of 8, 9, 12 mg/dl (1.06 mmol/L) or even higher. IRIS does not have criteria beyond the relatively low creatinine value of 5.0 so it is best to think of the IRIS system as a way to intervene in the earlier stages of renal insufficiency. For patients in more dire initial states, the goal is to drive their toxin levels down to where the IRIS system becomes relevant.
| Stage I (pre-failure) | Stage II (mild failure) | Stage III (moderate failure) | Stage IV (severe failure) | |
| Dog | <1.4 | 1.4 – 2.0 | 2.1 – 5 | >5 |
| Cat | <1.6 but SDMA >14 mcg/dl | 1.6 – 2.8 | 2.8 – 5 or SDMA >25 mcg/dl | >5 or SDMA >45 mcg/dl |
These stages are based on blood creatinine levels measured in mg/dl as well as SDMA measured in mcg/dl. There are no SDMA levels for Stage II.
Sub-staging of kidney disease involves screening for urine protein loss and measuring blood pressure. A urine protein:creatinine ratio is performed on a urine sample and the protein amount is classified as either non-proteinuric, borderline proteinuric, or proteinuric. Blood pressure is checked and the patient is classified as normotensive (normal), borderline hypertensive, hypertensive, or severely hypertensive. The ultimate classification for the patient will reflect all of these things (an example would be “Stage 3, non-proteinuria, normotensive”). Further testing and monitoring is determined based on what the actual parameters are. For more details on these see glomerular disease and hypertension.
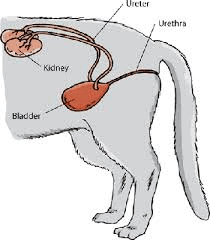
A Note on Pyelonephritis
Pyelonephritis is another name for kidney inflammation and usually means kidney infection. Patients get kidney infections when a bladder infection goes unnoticed or incompletely treated long enough and the bacteria ascend up the ureters into the kidney where they set up shop and cause damage and pain. This form of kidney failure has the most potential for reversal or partial reversal so it is important to culture the urine early. Urinalysis is frequently unable to detect infection in this situation as the patient drinks so much water that the visible markers of infection are diluted out and cannot be found. The infection also will produce a significant amount of urinary protein so the patient will be sub-staged incorrectly if infection is not ruled out.
The bottom line is that there is a wide range of what is involved when a patient has kidney failure or insufficient kidneys. Each patient will have a different stage and a different constellation of issues to contend with. Some will need only a diet change and some will need on-going fluid therapy at home or hospitalization. Prognosis depends on all the factors involved. Your veterinarian will let you know what your particular pet needs and will be watching many different lab tests to keep control of your pet’s condition.


