Is ringworm a worm?
Ringworm got its name because of the circular somewhat red worm-y pattern it makes on the skin of an infected individual from people to cats to dogs. Despite having some worm-like attributes, ringworm isn’t caused by a worm but is a fungal infection.
The fungi involved are called dermatophytes, and the more scientifically correct name for ringworm is dermatophytosis. The dermatophyte fungi feed upon the dead cells of skin and hair causing in people a classic round, red lesion with a ring of scale around the edges and normal recovering skin in the center. Because the ring of irritated, itchy skin looked like a worm, the infection was erroneously named.
The characteristic ring appearance is primarily a human phenomenon though.
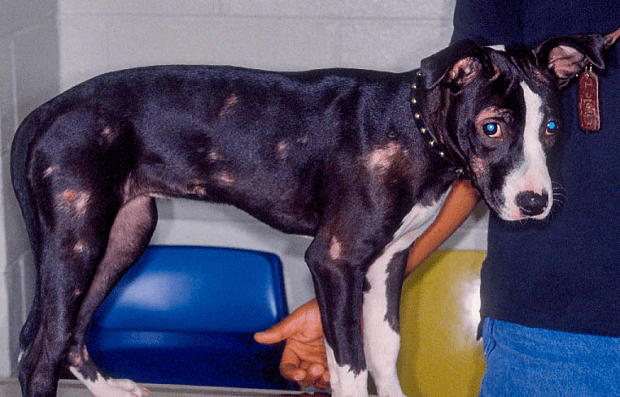
In animals, the classic appearance is a circular red rim that sometimes looks a little scale-y with loss of fur growth in the region.

That said, while the above is the classic appearance, it may also look like scabs or just areas of hair loss, making a definitive diagnosis by visual examination impossible as it can resemble other skin infections including bacteria, yeast or mange.
Where Does Ringworm Come From?
Ringworm fungi produce infectious spores that are stable in the environment for long periods of time. For a person or animal to become infected it requires a small wound or break in the skin barrier to come in contact with a spore.
The immune status of any individual that comes in contact with an infectious spore plays a role as well in whether an infection will occur. In companion animals, puppies and kittens are more likely to get infected due to their underdeveloped immune system.
Where would my pet pick up this Infection?
The spores of dermatophyte fungi are extremely hardy in the environment; they can live for years. All it takes is skin contact with a spore to cause infection; however, the skin must be abraded as the fungus cannot infect healthy intact skin. This means that freshly shaved, scraped, or scratched skin is especially vulnerable.
Infection can come from direct contact with an infected symptomatic animal, direct contact with an asymptomatic carrier, or contact with spores in the environment. Infected symptomatic animals have skin lesions rife with fungal spores.
Carriers may be infected animals who do not have obvious lesions (a common scenario towards the end of treatment) or they may be animals who are not actually infected per se but simply have spores on their hairs, just as a couch might have spores on its surface. Infection is transmitted when spores bind to abraded skin. Skin lesions typically appear one to three weeks after exposure.
There are several species of dermatophyte fungi. Different species come from different kinds of animals or even from soil, thus determining the ringworm species can help determine the source of the fungal infection. Predisposing factors towards infection include age (puppies and kittens are at higher risk than adult animals), life-style (free-roaming or hunting animals being predisposed), and local climate (pets living in warmer, more humid climates are predisposed).
Immune suppression from the FIV or Feline Leukemia Virus turns out not to be a predisposing factor as one might expect, especially since immune suppression is a human risk, but there are two breed predispositions of note: Persian cats and Yorkshire terrier dogs. Infection rates are higher in these breeds as are treatment failures.
People can get Ringworm, Too

Yes, ringworm is contagious to people; however, some people are at greater risk than others. Just like cats and dogs, the immune status comes into play. People that are immuno-suppressed from disease or medication are at a higher risk.
This puts pregnant women, elderly people, those who are HIV-positive, people on chemotherapy or taking medication after transfusion or organ transplant, and highly stressed people at high risk. Children also are at a higher risk for the same reasons puppies and kittens are.
In general, if you do not already have ringworm at the time your pet is diagnosed, you probably will not get it. Keep in mind that skin must be irritated to become infected.
Diagnosis
If you think your pet has ringworm, bring your animal companion to your veterinarian. While certain lesions look suspicious, especially if another pet or person in the household has it, often diagnostic testing is needed to be certain.
Veterinarians used to test with a fluorescent lamp called a Wood’s Lamp that emits a sort of black light. The misconception is that this is accurate. In truth, of the two commonly found ringworm species only one seems to show with the Wood’s lamp.
And even when it lights up, only 50% seem to emit a fluorescent glow. Additionally, other debris can also glow leading someone to misdiagnose what is really just skin cells or bacteria. For this reason, the Wood’s lamp is not a very good diagnostic tool.
Until recently, veterinarians took fur from affected regions and placed them on a culture medium to see if ringworm would grow. While this test is accurate, it can take up to three weeks so not as good for making a diagnosis quickly.
Microscopic Examination
Your veterinarian may wish to examine some hairs for microscopic spores. This involves plucking hairs and inspecting them under the microscope. If spores can be seen on damaged hairs, then the diagnosis of ringworm is confirmed; however, as spores are difficult to see, especially in darker hair, many veterinarians skip this step.

Positive Ringworm Culture
Also, this is the only test that is helpful in determining if animal is an asymptomatic carrier. The other tests require an apparent skin lesion to test. A pet with no apparent lesions can be combed over its whole body and the fur and skin that are removed can be cultured. Carrier animals are usually cats living with several other cats.
Fungal Culture
Some hairs and skin scales are placed on a culture medium in an attempt to grow one of the ringworm fungi. The advantage of this test is that it not only can confirm ringworm but can tell exactly which species of fungus is there. Knowing the identity of the fungus may help determine the source of infection. The disadvantage, however, is that fungi require at least 10 days to grow out. Unfortunately, false negative cultures are not unusual.
A specific growth medium, called dermatophyte test medium, is commonly employed to distinguish ringworm fungi from other fungi. Ringworm fungi classically produce a white fluffy colony and will turn the orange growth medium red within two to 14 days. When the colony is mature, material can be harvested from it and examined under the microscope for ringworm spores.
PCR Testing
Recently, labs have started offering PCR (polymerase chain reaction) testing (DNA amplification) and pair this with a culture. PCR tests can be performed on either tissue or hair samples and is sensitive in its ability to detect spores. This type of testing detects DNA from any fungi that can cause ringworm in pets. Problems with the test are that it will detect spores that are there incidentally so that the patient may have a skin disease other than ringworm but still test PCR positive if spores are innocuously present.
The benefit is PCR takes only days to complete leading to a faster diagnosis.
Biopsy
For highly atypical presenting cases, a biopsy may be needed. This is less common but it is an option if test results are inconclusive.
Sometimes the lesions on the skin are so uncharacteristic that a skin biopsy is necessary to obtain a diagnosis. Fungal spores are quite clear in these samples and the diagnosis may be ruled in or out. Depending on the outcome of preliminary tests, your veterinarian may begin ringworm treatment right away or postpone it until after more definitive results are available.
Treatment – the Pets and the Environment
Treating the pets and keeping the environment clean and free from infectious spores in essential to a good treatment outcome. Also treating to the point of two successive negative cultures is required to ensure the infection has been completely knocked out.
Topical Shampoos
Topical Shampoos are very helpful in reducing infectious spores. In the past there where very smelly lime-Sulphur dips. Today, we luckily have some formulated shampoos that work very well in killing spores. Miconahex + Triz has an anti-fungal and a disinfectant that is very helpful in reducing spores. It also smells nice and animals tolerate this much better than the older dips.
Ringworm Cream
If an animal only has one or two lesions and is immuno-competent, in some instances adding a ringworm cream containing clotrimazole or miconazole may work.
Oral Medication
In the majority of cases an oral anti-fungal is needed in addition to shampooing. Oral medication provides the foundation of ringworm treatment as it renders the fungus unable to reproduce and spread. With the spread of infection controlled, only the pre-existing fungus remains and generally can be removed with topical therapy as described later on.
Labwork is often required as many of these oral medications can cause liver problems, so it is important to monitor your pet while they are treated.
Currently, two medications are primarily recommended to treat ringworm: Itraconazole and terbinafine. Griseofulvin is also available and has been the traditional anti-ringworm oral medication for decades. It is still as effective as the other medications but the newer products appear to be safer and griseofulvin is rapidly becoming a historical note only.
Treatment with oral medication typically should not be discontinued until the pet cultures negative. Stopping when the pet simply looks well visually frequently invites recurrence of the disease.
Environmental Treatment
This article is reviewing the infection, diagnosis and treatment. But environmental decontamination is also important to prevent spread in your household and re-infection. Please use the link below to view an article from VeterinaryPartner that reviews cleaning the environment.
https://veterinarypartner.vin.com/default.aspx?pid=19239&id=7058488
Please note, this article is directed for pet owners on how companion animals are typically diagnosed and treated. If you or another person in your household think you are infected, please see a human dermatologist or medical provider.


