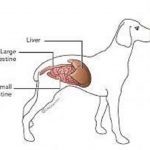
Pancreatitis is Inflammation of the Pancreas
In pancreatitis, inflammation disrupts the normal integrity of the pancreas. Digestive enzymes are normally stored safely as inactive forms within pancreatic granules so that they are harmless. In pancreatitis they are prematurely activated and released internally, digesting the body itself. The result can be a metabolic catastrophe. The living tissue becomes further inflamed and the tissue damage quickly involves the adjacent liver. Toxins released from this rampage of tissue destruction are released into the circulation and can cause a body-wide inflammatory response.If the pancreas is affected so as to disrupt its ability to produce insulin, diabetes mellitus can result; this can be either temporary or permanent.
What Causes Pancreatitis, Houston Heights
In most cases we never find out what causes it, but we do know some events that can cause pancreatitis.
Backwash (reflux) of duodenal contents into the pancreatic duct. The pancreas has numerous safety mechanisms to prevent self-digestion. One mechanism is storing the enzymes it creates in an inactive form. They are harmless until they are mixed with activating enzymes. The strongest activating enzymes are made by duodenal cells which means that the digestive enzymes do not actually activate until they are out of the pancreas and mixing with food in the duodenum. If duodenal fluids backwash up the pancreatic duct and into the pancreas, enzymes are prematurely activated and pancreatitis resuls. This is apparently the most common pancreatitis mechanism in humans, though it is not very common in veterinary patients.
Concurrent hormonal imbalance predisposes a dog to pancreatitis. Such conditions include: Diabetes mellitus, hypothyroidism, and hypercalcemia. The first two conditions are associated with altered fat metabolism, which predisposes to pancreatitis, and the latter condition involves elevated blood calcium that activates stored digestive enzymes.
Use of certain drugs can predispose to pancreatitis (sulfa-containing antibiotics such as trimethoprim sulfa, chemotherapy agents such as azathioprine or L-asparaginase, and the anti-seizure medication potassium bromide). Exposure to organophosphate insecticides has also been implicated as a cause of pancreatitis. Exposure to steroid hormones have traditionally been thought to be involved as a potential cause of pancreatitis but this appears not to be true.
Trauma to the pancreas that occurs from a car accident or even surgical manipulation can cause inflammation and thus pancreatitis.
A tumor in the pancreas can lead to inflammation in the adjacent pancreatic tissue.
A sudden high fat meal is the classic cause of canine pancreatitis. The sudden stimulation to release enzymes to digest fat seems to be involved.
Obesity has been found to be a risk factor because of the altered fat metabolism that goes along with it.
Miniature Schnauzers are predisposed to pancreatitis as they commonly have altered fat metabolism.
Signs of Pancreatitis, Houston Heights
The classical signs in dogs are appetite loss, vomiting, diarrhea, painful abdomen, and fever or any combination thereof.
Treating Canine Pancreatitis
The most important feature of treatment is aggressively rehydrating the patient with intravenous fluids as this restores the circulation to the pancreas and supports the natural healing mechanisms of the body. This means that the best route to recovery involves hospitalization. Fluids are continued until the patient is able to reliably drink and hold down adequate fluid intake, a process that commonly takes the better part of a week. Pain and nausea medication are needed to keep the patient comfortable, restore interest in food, and prevent further dehydration.
Plasma transfusion is somewhat controversial in treating pancreatitis. On one hand, plasma replenishes some of the natural blood proteins that are consumed by circulating digestive enzymes and would seem to make sense. In humans with pancreatitis, however, no benefit has been shown with plasma transfusion. Whether or not the protection afforded by plasma is real or theoretical is still being worked out but since it is difficult to go wrong with a plasma transfusion, do not be surprised if your veterinarian uses this approach.
In the past, nutritional support was delayed in pancreatitis patients as it was felt that stimulating the pancreas to secrete enzymes would encourage the on-going inflammation, but this theory has been re-thought. Currently, earlier return to feeding has been found to be beneficial to the GI tract’s ability to resume function. If nausea control through medication does not give the patient a reasonable appetite, assisted-feeding is started using a fat-restricted diet. Return of food interest and resolution of vomiting/diarrhea generally means the patient is ready for return to the home setting. Low-fat diets are crucial to managing pancreatitis and their use should be continued for several weeks before attempting return to regular dog food. Some dogs can never return to regular dog food and require prescription low fat foods indefinitely.