The term hemorrhagic gastroenteritis refers to inflammation of the stomach and intestine with bleeding. This kind of bleeding inflammation might be seen in patients with other issues including parvovirus, pancreatitis, inflammatory bowel disease and more.
However, when the term HGE is used, it usually refers to a more specific dog syndrome. HGE is a potentially life-threatening intestinal condition of an otherwise healthy dog, which manifests as sudden onset bloody, watery diarrhea. The result can be extreme dehydration from the amount of diarrhea, and if it is not promptly treated, the dog can go into shock and can die.
Vomiting is often part of the syndrome; in fact 80 percent of patients experience vomiting approximately before the dramatic bloody diarrhea and about half the time vomiting contains blood. The good news is that with fast hospitalization and treatment, most dogs recover rapidly.
Smaller dogs seem to have a predisposition towards HGE though any dog can be affected. Stress and hyperactivity seem to be predisposing factors.

with this condition
How is this Condition Diagnosed?
There are no specific tests for HGE but a test called a packed cell volume (also called PCV or hematocrit) is helpful in making the diagnosis. This test can be performed by your veterinarian. The percentage of the blood volume made up by red blood cells is measured.
A normal PCV for a healthy dog would be 37-55 percent, meaning 37-55 percent of the blood volume should be red blood cells; the rest is fluid and white blood cells. When the patient becomes really dehydrated, there is less fluid in the bloodstream and the percentage of blood increases. Basically, a veryy dehydrated patient has a very high PCV.
The average HGE patient will have a PCV of at least 57%. (It will even be greater than 60% in many patients.)
The measurement of the PCV also usually includes some sort of measurement of total protein (sometimes called total solids). In AHDS, the total protein measurement from the blood sample is paradoxically normal or low.
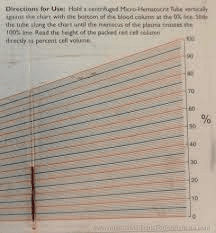
measured where the blood ends on
the chart line
Elevated PCV of 57% or more
There are several aspects to the HGE syndrome and they do not all have to be there to make the diagnosis. The syndrome elements your veterinarian will be looking for are:
- Relatively low total protein
- At least one episode of vomiting (with or without blood)
- A watery, very bloody diarrhea that looks almost like pure blood
- Relatively young dog (median age is five years)
- Relatively small dog (median size 25 lbs)
- Rapid response to intravenous fluids
As noted, there are many causes of a bloody diarrhea like this, including intestinal foreign body that requires surgery. Expect your veterinarian to need other tests to rule out other potentially more serious conditions.
What Causes HGE?
There are still many unknown factors but the cause appears to begin with infection from an intestinal bacterium called Clostridium perfringens Type A. A PCR test for Clostridium perfringens Type A can be used to determine for sure. This organism produces two toxins that is well known to cause diarrhea. The toxin ulcerates the intestinal lining and the intestinal blood vessels become permeable to fluid. In this way, fluid is lost into the intestine dehydrating the patient and the PCV rises while the ulcers are responsible for the bleeding.
Treating HGE
The heart of therapy is aggressive fluid replacement. The idea is to get the PCV back to the normal range and keep the patient out of shock. Medication for nausea and pain control are included as is a low fat diet as soon as the patient is willing to eat. As dramatic as the diarrhea is, most patients have an equally dramatic improvement in the first 24 hours of hospitalization and the average dog is out of the hospital after three days total.
Antibiotics are surprisingly controversial in this syndrome and their use depends on many patient factors (such as whether or not there is a fever, white blood cell count, whether or not the expected improvement is achieved, etc. It is not uncommon to use a drug called metronidazole which reduces intestinal inflammation and also kills Clostridium bacteria.
Stool can be expected to gradually return to normal over the course of about one week.
Probiotics (cultures of healthy bacteria) have been recommended to help repopulate the bowel but it is best to start these after recovery is well underway and the intestinal ulcers have healed.


