
If you have found your way here, you probably have a pet who has been diagnosed with chronic kidney failure or insufficient kidney function and you want to know what that means and what you should be doing to return your pet to health or to maintain your pet in good condition. In fact, the kidneys do many things besides simply eliminating toxins in urine and when the kidneys become diseased there may be several functions they can no longer maintain. We have information to help you understand what is happening and what you can do about it.
Kidney Failure, Chronic Renal Failure, Renal Insufficiency and Insufficient Kidney Function
All of these terms mean the same thing: the kidneys can’t keep up with their daily work. In the past, kidney failure was the predominant term but as these words conjure up images of on-going sickness, expensive hospitalization, and doom they have been largely put aside for terms such as renal insufficiency and insufficient kidney function. After all, loss of kidney function can be mild, moderate, or severe. Recommended treatment is different depending on which jobs the kidneys are not keeping up with and how bad the function loss actually is.
The purpose of this article is to review the parameters involved in renal insufficiency so that you will understand what your veterinarian is monitoring and why. We will also review the stages of kidney failure as defined by the International Renal Interest Society so that you can know where your pet stands and how fast or slow your pet’s condition is progressing. Obviously, the goal is to keep the pet feeling completely normal and slow or arrest the disease’s progression.
Before reviewing what failing kidneys can no longer do, it is important to know what normal kidneys do. Kidney function goes far beyond simply making urine. Kidneys are made of millions of processing units called nephrons. These tiny little processing units are responsible for separating the chemicals you want to keep in your body from the chemicals you need to discard. The chemicals to discard are dissolved in water and make up the fluid we all know as urine. So here are the tasks your kidneys perform for you and your pet. Insufficient kidneys lose the ability to do some of these tasks but usually manage to keep up others. When one function becomes a problem, we can usually help with diet or medication.
What our Kidneys Do / What Insufficient Kidneys Cannot Do
Water Conservation
Hydration of the body depends not only on water consumed but on water removed. In times of dehydration, the kidney must respond by conserving water. This means that all the materials that the body needs to get rid of still need to removed, but the kidney needs to manage this feat using the smallest amount of water possible. Similarly, if you drink too much water, the kidney needs to efficiently remove the excess to prevent dilution of the blood stream. A pet with insufficient kidney function will not be able to make a concentrated urine and will need to drink extra water to process the body’s waste chemicals. For this reason, excessive water consumption is an important early warning sign and should always be investigated.
Toxin Removal
When we analyze a urine sample, one of the most important parameters is the specific gravity, a measure of how concentrated a urine sample is. Water has a specific gravity of 1.000. A dilute urine sample has a specific gravity less than 1.020 (often less than 1.015). A concentrated urine sample would have a specific gravity over 1.030 or 1.040. A failing kidney by definition cannot make a concentrated urine and the patient must drink excessively to get enough water to excrete the day’s toxic load.
The kidneys remove our metabolic wastes for us. If there is inadequate circulation going through the kidneys or if there are not enough functioning nephrons to handle the waste load, toxins will build up. When they build up and exceed the normal range, a condition called azotemia exists. If the toxins build up to a level where the patient actually feels sick, a condition called uremia exists. If we can keep our azotemic patient below the uremia level, she will feel pretty normal and have good life quality.
There are three markers of azotemia and uremia: creatinine, SDMA (symmetrical dimethylarginine), and BUN (blood urea nitrogen). For decades, creatinine has been the chief marker. Creatinine is a by-product of muscle break-down and is always in the bloodstream in small amounts. The kidney removes it continuously unless there is a kidney function problem. How much creatinine is in the bloodstream correlates to the kidney’s ability to remove toxins and allows for renal insufficiency to be staged. If the patient is very skinny, creatinine can be falsely lowered, so body condition is also a factor in monitoring creatinine. (Remember, creatinine comes from muscle so if there isn’t a lot of muscle, there is less creatinine.)
SDMA is a newer parameter and its elevation similarly relates to the kidney’s ability (or lack thereof) to remove toxins. SDMA becomes abnormal much sooner than creatinine and allows for an earlier detection of loss of kidney function.
BUN is another marker with similar implications to toxin removal; however, BUN is influenced by dietary protein levels (or the presence of intestinal bleeding). BUN usually elevates in proportion to creatinine but not always.
These three parameters are considered to determine how advanced the renal insufficiency is. It is important to note, however, that dehydration will raise all three of these parameters so the true renal stage will not be evident until the patient is rehydrated.
Calcium/Phosphorus Balance
The balance between calcium and phosphorus in the blood is important. Too much of one or the other will lead to crystals forming in the tissues of the body and weakening of the bones to the extent they may actually become rubbery. The kidney plays an important role in this balance and when kidney function is lost, phosphorus levels begin to rise. Therapy for insufficient kidney function requires monitoring of phosphorus levels and the use of diet and medications to keep phosphorus levels in a reasonable range.
Sodium/Potassium Balance
The kidney plays a major role in controlling electrolyte balance as well. In particular, conservation of potassium is an important aspect. Insufficient kidneys lose their ability to conserve potassium and potassium levels begin to drop leading to weakness. Potassium supplements are commonly needed in the treatment of kidney failure.
Blood Pressure Regulation
Blood pressure sensors in the kidney help regulate blood pressure in the body. When these are damaged, hypertension (high blood pressure) can result and can damage the kidney further. Blood pressure is commonly measured in kidney failure patients.
Protein Conservation
There are a lot of important proteins circulating in the bloodstream and it is crucial that they are not lost in urine. The nephron possesses a filtration system that keeps protein in while removing harmful wastes. If this filtration system is damaged (glomerular disease) then a much more severe form of kidney failure results. Screening for this damage is an important aspect of staging kidney failure and a test called a urine protein:creatinine ratio is often included in the testing profile to assess this condition.
Red Blood Cell Production
The kidney produces a hormone called erythropoietin. This hormone tells the bone marrow to make more red blood cells. In the absence of this hormone, a non-responsive anemia occurs and can get so bad that transfusion is necessary. Erythropoietin can be given by injection to alleviate this problem but there are some potential pitfalls in doing this. Hematocrit and PCV (packed cell volume) are measures of red blood cell volume that are commonly monitored in kidney patients.
pH Balance
Metabolic processes require a narrow pH range for efficiency. The kidney also regulates this balance and if it cannot, intervention is necessary, usually in the form of fluid therapy.
Staging and Sub-Staging
We are born with two kidneys and a huge excess of nephrons. As we live our lives, nephrons die off either as a consequence of disease or simply through wear and tear. When we are down to less than one-third of our kidney’s worth of nephrons (in other words we have lost 5/6 of our total nephrons), test results become notably abnormal and it becomes important to make lifestyle changes. How big these changes are depends on how far things have gone out of whack when the problem is discovered. Early detection of poor kidney function is one of the main reasons laboratory screening tests are recommended.
A Note on Pyelonephritis (infection of the kidneys)
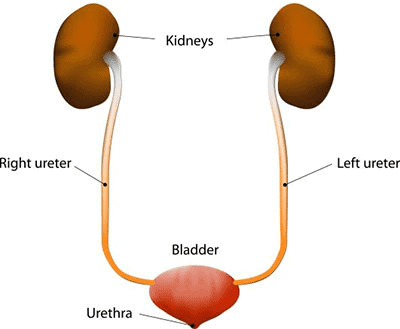
Pyelonephritis is another name for kidney inflammation and usually means kidney infection. Patients get kidney infections when a bladder infection goes unnoticed or incompletely treated long enough and the bacteria ascend up the ureters into the kidney where they set up shop and cause damage and pain. This form of kidney failure has the most potential for reversal or partial reversal so it is important to culture the urine early. Urinalysis is frequently unable to detect infection in this situation as the patient drinks so much water that the visible markers of infection are diluted out and cannot be found. The infection also will produce a significant amount of urinary protein so the patient will be sub-staged incorrectly if infection is not ruled out.
The bottom line is that there is a wide range of what is involved when a patient has kidney failure or insufficient kidneys. Each patient will have a different stage and a different constellation of issues to contend with. Some will need only a diet change and some will need on-going fluid therapy at home or hospitalization. Prognosis depends on all the factors involved. Your veterinarian will let you know what your particular pet needs and will be watching many different lab tests to keep control of your pet’s condition.


