About the Organism
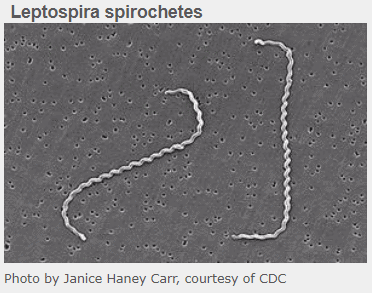
Leptospira organisms are spiral-shaped bacteria called spirochetes. There are several species of leptospires, but the ones that cause disease have been grouped into one particular species. From here, over 250 strains have been named and at least 10 are important for causing disease in pets, especially dogs. Canine vaccine for dogs, however, exists against only four serovars (strains). These have been the four most commonly identified serovars in infected dogs. Different serovars produce different types of disease and are in different geographical areas.
Strains or Servovars
- Canicola – This serovar is the most common in Mexico. It produces primarily kidney disease. With a constant influx of dogs across the border, this is a serovar to watch for in particular.
- Pomona – This serovar has an association with livestock and tends to produce severe disease in both the kidney and liver.
- Grippotyphosa – In a survey of over healthy 1200 dogs in Michigan, 24% of dogs tested as exposed to Leptospira and the Grippotyphosa serovar was the most common.
- Leptospires live best in warm, slow-moving water such as after heavy rains or flooding. After the water clears, they contaminate soil for many months. Wildlife are common carriers of infection. A survey in Connecticut found 36% of racoons had been exposed while a survey in Illinois found 48% of raccoons had been. Another survey found 50% of rats had been exposed. Classically, infection of dogs and humans stems from the urine of infected animals getting into environmental water. Leptospirosis is a common human disease in tropical areas, especially where rice is farmed and rats infest the paddies. It is believed that rat populations are involved in the rising incidence of canine leptospirosis in urban areas, and leptospirosis is no longer considered a rural disease. Leptospires can survive for months in contaminated soil.
Canine Infection
Dogs become infected by leptospires when irritated or cut skin comes into contact with infected urine or water contaminated with infected urine. Alternatively, bite wounds, exposure to reproductive secretions, and even eating infected tissues can transmit this infection. The organisms quickly spread through the bloodstream, leading first to inflaming the blood vessels themselves: fever, abnormal bleeding, abnormal bruising and tissue edema appear after an approximately 7-day incubation period.
By 2 weeks post-infection, the leptospires have set up shop in the kidneys where they continue to generate inflammation, pain, and potentially total kidney failure with their inability to produce urine. Some serovars also go to the liver and generate inflammation there, though the liver disease is generally not as severe as that of the kidney.
A particularly devastating situation occurs if the organism gets into the lungs where the leptospire toxins produce what is termed “Leptospira Pulmonary Hemorrhage Syndrome.” The lung bleeding that results is associated with a 70% mortality rate and bodes especially poorly.
If the dog is able to keep the acute illness at bay, a chronic form may emerge. There can be a more chronic kidney insufficiency and/or hepatitis. Furthermore, the long-term immune stimulation can lead to a deep eye inflammation called uveitis that can cause the eyes to look cloudy or even change color. If the disease is treated in this form, it may not be possible to reverse the long-term damage that has already set in.
The Different Clinical Pictures of Leptospirosis
As you might gather, leptospirosis can look different: fever with bruising and bleeding; fever with different degrees of kidney failure; liver disease and kidney disease together; chronic hepatitis; and eye inflammation etc. Another way to look at leptospirosis is to look at the time frame of the illness and how quickly or slowly it came on.
Peracute Disease: Peracute disease means super-sudden onset. These are usually younger dogs with an overwhelming exposure. The large amount of leptospire toxin causes rapid death before the kidney or liver disease even happens.
Acute Disease and Subacute Disease: This is more the classic form described above: fever with bruising and bleeding, general muscle pain, painful belly from the kidney and/or liver disease. There may be jaundice and inflammation in the eyes that makes them look cloudy.
Chronic Disease: Recurring fevers, chronic hepatitis, chronic kidney disease, uveitis, poor appetite, weight loss.
Younger dogs (less than 1 year of age) tend to get the most severe forms of leptospirosis.
87-100% of infected dogs will have some degree of kidney impairment found in routine blood and urine testing.
Testing

PCR Testing
PCR testing is used to detect leptospire DNA. A blood sample is best in the first 10 days after infection, but after that a urine sample is more likely to be positive. It may be prudent to submit both blood and urine samples. Past vaccination will not interfere with this test, although antibiotic exposure certainly will, and results can be back in a day or so. PCR testing will not determine which serovar is present.
Antibody testing – MAT Testing (the Traditional Test)
The Microscopic Agglutination Test or MAT test is still considered the test of choice though it has some disadvantages. It measures antibody levels against different Leptospirosis serovars with the idea being that the one with the highest level is most likely to be the serovar causing the disease.
Antibody levels are expressed as titers, which are ratios reflecting how much dilution is needed before it is too dilute to detect antibodies. For example, a titer of 1:32 means a serum diluted out 32 times still had detectable antibody.
A titer of 1:32 may sound pretty high but it is actually pretty low; an MAT titer must be at least 1:800 to be considered positive. If the serovar under consideration has an associated vaccine, a titer more like 1:3200 is considered positive.
To really obtain high confidence in the diagnosis of Leptospirosis, a second titer is submitted 2-4 weeks later showing at least a four-fold increase in antibody production. Treatment with antibiotics should not interfere with the validity of the second (or “convalescent”) titer level.
There are two problems with this testing:
- No one wants to wait 2-4 weeks to confirm the diagnosis especially with a disease contagious to humans. PCR testing gets results much faster.
- Vaccination interferes with results (remember the entire goal of vaccination is to generate an antibody titer). Vaccination history can make interpretation difficult.
Treatment
Fortunately, Leptospira interrogans sensu lato is sensitive to doxycycline, a readily available antibiotic. Leptospires are cleared from the blood within 24 hours of starting antibiotics but it takes about a week for them to clear from the urine, so it is important for you to wear gloves, goggles, etc. and be conscious of contamination.
Intravenous fluids are crucial to support blood flow through the damaged kidneys so that recovery is possible. Any areas at home that have been contaminated with urine should be disinfected with an iodine-based product and gloves should be worn while cleaning up any urine. Prognosis is guarded depending on the extent of organ damage; with appropriate treatment, 80-90% survival rates are reported.
This sounds wonderful but it is important to keep in mind factors that can interfere with this rosy outcome. While most leptospirosis-related kidney injury responds to fluid therapy as can be given by most animal hospitals, more severe cases can require dialysis, which has limited availability. As mentioned, lung involvement has very poor surviviability. Infection with the Pomona serovar is associated with more severe disease.
A good two weeks of doxycycline is generally needed. If this antibiotic is not tolerated, amoxicillin may also work.
Prevention
Vaccination against Leptospira interrogans sensu lato is only available for the serovars called Canicola, Grippotyphosa, Pomona and Icterohaemorragiae. (Some vaccines cover all four serovars while others cover only two out of four.) As a result of long-standing use of this vaccine, it is hard to assess how important it is to vaccinate against leptospirosis. As you might imagine, some outbreaks involve serovars for which vaccination does not exist, which, while unfortunate, also suggests that the vaccine is working.
Vaccination against Canicola and Icterohaemorragiae has been traditional for dogs as it is included in the basic distemper shot (DHLPP – the “L” stands for leptospirosis). The American Animal Hospital Association vaccine guidelines consider vaccination against leptospirosis to be optional but recommends that if you are going to vaccinate for leptospirosis, use a vaccine covering all four serovars.
In the past, leptospirosis vaccine was felt to be associated with a higher chance of immunological vaccine reactions, but newer vaccines made from leptospires grown in protein-free media have made vaccination reaction far less likely.
Vaccination will reduce the severity of disease but will not prevent infected dogs from becoming carriers.
Other important aspects of prevention include controlling rodents in the pet’s environment and removing standing water.
Other Things to Note:
While most infections result in elevated kidney and / or liver values, it is important to note that this disease can cause a range of symptoms that may be less straightforward especially in the absence of bloodwork changes.
In some cases patients present with loss of appetite, reluctance to stand (muscle pain) and the only labwork abnormality may be very dilute urine. Your veterinarian should be able to help you make a diagnosis after examining your pet, reviewing labwork and may recommend PCR and antibody testing.
Leptospirosis is Zooinotic – it can be passed to Humans
The Centers for Disease Control and Prevention monitors leptospirosis cases in people, it seems that one third come from contact with infected dogs and one third come from contact with rats (usually through field work). Recreational activities involving water and exposure to flood waters are also associated with human outbreaks. Other human risk factors include farm work, animal care work, camping, and sewer work. Remember, leptospires come from contaminated urine which, in turn, contaminates environmental water and soil.
The same symptoms occur in humans as would be seen in dogs.