Dog Anal Gland Tumors

Many dog owners have seen their companion scoot their rump across the floor in a disconcerting way. Sometimes you may smell a fishy odor or see brown droplets after the scoot. If you have, your dog’s anal glands were probably full and itchy, making your pet rub and also try to empty their glands. People also have anal glands but ours don’t fill up and we don’t use it to mark territory. Ours are more small remnants that are not significant. In dogs it’s a different story. What are anal glands and where are they? Anal glands are basically small sacs located just inside the rectum on each side. On the left between the 6-7 o’clock position and on the right between 4-5 o’clock. There are pores to the gland. Normally, every time your dog defecates the glands are pressed and emptied. However, some dogs have small pore openings or conditions that inflame the gland and make them hard to empty; that’s when they scoot. This liquid may play a role in territorial marking and communication between our canine friends. While anal glands can be emptied by your veterinarian, there are other problems that can occur in the glands. One such problem are tumors. Anal sac tumors are abnormal, usually cancerous growths in the gland. They are not too common but serious and left untreated are generally fatal. These tumors can affect any dog but older dogs and certain breeds such as spaniels, German Shepherds, and dachshunds are at higher risk. Females seem to be affected more frequently than males. These tumors can metastasize and create issues as they spread locally and to distant sites of the body. Ultimately, they can bring illness, discomfort and a decreased quality of life to your dog. For this reason, it is essential to catch these tumors early and to treat them as soon as possible. What causes anal sac tumors? As with most cancers, a cause has not been identified. However, genetics and environmental factors probably play important roles. Although we don’t have a definite cause, we do have some understanding of what’s happening at a microscopic level. As in most tumors, cells start abnormally dividing and multiplying in an unregulated way. This rapid cellular replication creates a cancerous. The mass makes the anal sac larger and can get large enough that defecation becomes difficult. More trouble follows when cancer cells spread to other parts of the body and make new tumors. The cells often spread to lymph nodes, which are small lumps of immune tissue scattered throughout the body. They can also spread to essential organs, such as the lungs, liver and kidneys. The other problem caused by anal gland cancer is this type of tumor is often implicated in dysregulation of calcium metabolism in the body and may cause increased the amount of calcium in the blood. High calcium levels can damage the kidneys as well as cause muscle tremors, heart beat abnormalities and increased thirst and urination. Early signs of anal sac tumors early on, many dogs won’t show any signs. They may scoot however just like when their glands are full. If your veterinarian checks, he or she may feel the mass and recommend obtaining a sample for pathology. If the tumors are not caught early, you may notice that your dog is having trouble defecating. If the tumor increases blood calcium levels, your dog may drink and urinate more, tremble, vomit and seem weak. If the mass spreads to the lungs, owners may hear coughing. Other symptoms include: How are anal sac tumors diagnosed and treated? Your veterinarian will conduct a rectal exam to feel for the tumor. If a mass is suspected, your veterinarian will likely recommend sedated needle aspirations for clinical pathology. If it is determined to be cancerous, your veterinarian will recommend labwork, chest X-rays and an abdominal ultrasound to make sure obvious spread isn’t seen. If it isn’t, surgical removal (and in some cases radiation treatment) will be recommended. Until your dog is scheduled for treatment, your veterinarian may recommend stool softeners to make it easier for your dog to defecate and give medications to lower blood calcium. They may also refer you to a veterinary surgeon and oncologist for removal, radiation and chemotherapy if warranted. Surgery has been shown to lengthen the survival time of dogs with anal sac tumors. However, tumors may eventually reappear if cancer cells are left behind and the cancer cells may have already spread to other sites at the time of removal. Both chemotherapy and radiation therapy can have serious side effects that your veterinarian as well as veterinary specialists will talk to you about. What is the prognosis? Survival times for dogs with anal sac tumors are variable but on average range from about 1-2 years. However, every dog’s situation is different because prognosis depends on many factors such as: Dogs who receive surgery or any type of treatment generally have a better prognosis whereas the outlook is often much poorer for dogs with large tumors, higher calcium levels, and extensive spread of the tumor. How can I prevent anal sac tumors? There’s no way to prevent anal sac tumors from developing. Early detection is important and may be achieved through routine rectal exams performed by your veterinarian. In fact, many times anal sac tumors are found when your veterinarian does a rectal examination.
Grain-free Pet Diets and Heart Disease in Pets

You may have heard about a link between grain-free diets and canine heart disease from the news or from your veterinarian. If you haven’t, here’s some important information we’d like to share with you: The U.S. Food and Drug Administration has alerted pet owners and veterinary professionals about reports of canine dilated cardiomyopathy (DCM) in dogs that are eating grain free foods. It should be noted that cats eating similar foods are at an even greater risk. Canine dilated cardiomyopathy (DCM) is a heart muscle disorder that results in a decreased ability of the heart to pump blood through the body. Historically, this seemed to be a heritable disease affecting certain dog breeds. Previously, cats eating certain diets came down with this disorder. Once dietary changes were made by food companies, we stopped seeing this in cats and only specific dog breeds, most notably the Doberman Pincher, Boxers, Irish Wolfhounds and Great Danes. More recently, with the advent of grain-free / boutique diets, veterinary cardiologists began reporting the disease in atypical dog breeds. The FDA stated in its report in July that the Center for Veterinary Medicine is looking into the links between grain-free dog foods and DCM along with the Veterinary Laboratory Investigation and Response Network. Recently, veterinary cardiologists have been reporting increased rates of DCM in breeds not usually associated with DCM such as Miniature Schnauzers, Golden Retrievers, Labrador Retrievers, Doodle mixes, Shih Tzus and French Bulldogs. There is suspicion that the disease is associated with eating boutique or grain-free diets with some of the dogs improving when their diets are changed. A cardiologist from North Carolina State College of Veterinary Medicine noted DCM in a household with two unrelated Miniature Schnauzers and they were both eating the same boutique, exotic protein grain free diet. Cardiologists have noticed that both the typical and atypical breeds were more likely to be eating boutique or grain-free diets with ingredients such as kangaroo, lentils, duck, pea, fava bean, buffalo, tapioca, salmon, lamb, barley, bison, venison, and chickpeas. Some vegan diets have been associated with DCM and it has even been seen in dogs eating raw or home-prepared diets. The cause of the rise in DCM in breeds not usually associated with this condition is unclear at this time. The most likely opinion is related to the amino acid taurine. While most grain-free foods have it, there may be a problem with how its processed and absorbed in the grain-free diets. Taurine is an essential amino acid involved in heart contractility. We learned this lesson the hard way when DCM was found in cats. In 1987 it was discovered that feline DCM was caused by insufficient taurine in the diet. All reputable commercial cat foods now contain enough taurine to prevent the development of this lethal disease. While no one is 100% certain why the grain-free diets are causing DCM, it is suspected that there is a link to how the taurine is processed. Most of the atypical dogs affected were eating boutique, grain free or exotic ingredient diets. Many affected dogs improved with taurine supplementation and returning them to a traditional grain diet. If you are feeding your dog or cat a grain-free or raw diet, it is recommended that you switch back to a traditional grain fortified diet. In fact, there is no proven benefit to feeding a diet that lacks grains. So what is the best diet for your pets? You can speak with your veterinarian about what diet is most appropriate. based on your pet’s age, level of activity, and any special needs or requirements they may have. The right nutrients in the right proportions must be in the diet, the effects of processing (or not processing) the food needs to be considered, and the effects all the other ingredients in the food need to be addressed, in addition to ensuring rigorous quality control and testing. Not every manufacturer can do this type of quality control and food analysis/testing and certainly not every manufacturer does. If your pet is in good health and a good body weight, some very reputable brands that put a lot of research into their foods include Royal Canin, Hills, Eukanuba and Purina. These diets are readily available in pet food stores and some are even found in supermarkets.
Melanomas in Companion Dogs and Cats

Most people know about melanoma and know it is a skin cancer. It arises from pigmented skin from a pigmented cell type called melanocytes. In people melanomas are commonly associated with sun exposure and overexposure. Likewise, the situation in pets involves cancer of the melanocytes and pigmented growths. the difference is, in pets, specific body parts are classically involved. While you should tell your family veterinarian about any pigmented growth, there are specific areas on the body to be particularly concerned about. UV rays from the sun is less important. Benign Vs. Malignant Melanomas/Haired Skin Melanomas The behavior of a melanoma is highly dependent on where in the body it develops. Most areas of the skin grow benign versions of melanoma that are called melanocytomas. This means that a pigmented growth found on haired skin in an area that is not considered a danger zone is likely to behave benignly. That said, they do not all behave benignly, it is important to have all tumors analyzed by a pathologist so that a given tumor’s behavior can be predicted. What ancillary treatment or testing is recommended (if any) will be determined based on this tissue analysis. Many melanomas removed from haired skin show cells that look malignant under the microscope but do not behave in a malignant manner. To get a better sense of how a given tumor will behave, the number of cells in the process of division is counted in the sample. Often a veterinary pathologist will look at samples and use a number of criteria to determine if a mass is benign or is concerning for malignancy. There is some suspicion that haired skin melanomas developing within 1 cm of a mucosal margin (like the mouth or genital area) behave more aggressively. It is not wrong to have any growths sent out for pathology. In some cases, your veterinarian may refer you to a veterinary oncologist for further consult and treatment recommendations. Below are some areas that lead toward more aggressive behavior from melanomas: Each of these three scenarios is reviewed in more detail below: Melanoma of the Mouth Oral melanomas are very malignant. It is locally destructive in the mouth plus it readily and quickly spreads to other areas of the body. This means that there are three aspects of the cancer requiring attention: the local destruction; tumor cells that are spreading; along with the cancer detected in other organs besides the primary site of origination. Once a melanoma is confirmed, your veterinarian will stage the tumor to see how far it has spread (or not). Chest radiographs are used to screen metastasis to the lungs and local lymph nodes are sampled. In addition, an abdominal ultrasound is recommended to look for masses in the abdomen. Size Matters! In the mouth, the size of the tumor is extremely important when considering the prognosis. Veterinary medicine has adopted the World Health Organization staging system. Stage I disease is a tumor less than 2 cm (just less than 1 inch) in diameter; Stage II disease is a tumor 2 – 4 cm in diameter; and Stage III disease consists of tumors 4 cm or larger or any tumor with local lymph node involvement. Stage IV disease includes any tumor with evidence of distant spread. Median survival times for oral melanoma have been reported as: Additional therapies The goal of additional therapies such as radiation, chemotherapy, immunotherapy is to extend this time. In veterinary medicine, treatment is often not curative but can increase survival times. Toe melanoma Developing melanoma in the toe or toenail bed seems to be a particular problem for dark colored dogs. The tumor is particularly destructive to the bone and quite painful, starting usually as a swelling that seems associated with an infected toenail. The toe infection may improve with treatment but ultimately, the issue doesn’t resolve. If the tumor has not spread beyond the toe, amputation should be curative. Unfortunately, often by the time the diagnosis is made, many of these tumors have already spread. Because this is such an aggressive tumor, staging is important after melanoma is confirmed. This means chest radiographs, lymph node sampling, and ultrasound of the abdominal organs to identify distant spread. Ocular (Eye) Melanoma Uveal/Iris Melanoma – Dogs The pigments of the iris and ciliary body within the eye are especially vulnerable to melanoma development. These tumors are particularly difficult to see until they are fairly large. The clinical situation is different depending on whether the patient is a cat or a dog. The good news is that this is a benign condition in at least 80 percent of patients. In cases where progressive growth is seen, it is probably best to simply remove the eye (enucleation) though smaller growths might be amenable to laser therapy. Uveal/Iris Melanoma – Cats The feline situation is different. In cats, the majority of ocular melanomas are malignant and will spread. Tumors may start as flat areas of pigment on the iris (colored part of the eye) and progress to a 3D bulge. The eye will likely need removal to manage the pain from the expanding growth. Always remember, it is best practice to stage with x-rays, local lymph node sampling, ultrasound of the abdominal organs to ensure the tumor hasn’t spread. Iris melanosis, which is a benign condition, can be impossible to distinguish from an early melanoma so often periodic evaluation by a specialist is in order. Iris melanosis refers to the “freckles” and flat dark spots that older cats develop on their irises. These spots are common but should not have any bulging. Often a special light on an ophthalmoscope called a slit lamp can show if the spot is starting to bulge as the slit light will warp over a 3D surface. Epibulbar Melanoma This form of melanoma is usually benign in either dogs or cats and arises on the outer eye portion where the sclera (white part) meets the cornea (clear part over the iris). Smaller growths may not need
Rabies and Your Pet

Rabies has existed for a long time and is one of the most serious viral infections for people and mammals alike, as there are no second-chances. It is always fatal (with the exception of a case where a female was placed into a coma while her body had time to mount an immune response). The good news, is: The virus does not survive outside of the infected host very long. Direct contact from infected salvia or a bite is required for transmission. Most individuals get infected from an animal bite from wildlife harboring the infection such as a racoon, bat, or fox. However, in some cases, cats and dogs that become infected may spread it to their human companions. When wildlife starts coming into contact with the pet population, pets may become infected and then, human infection follows. Because Rabies infection has a 100% mortality rate, it is essential to prevent this in your cats, dogs and other mammalian household animals including ferrets. Common wildlife species that have the virus in North America are skunks, bats, raccoons, foxes, and coyotes. It can take many months for the virus to incubate and an individual to become symptomatic, but once even mild symptoms begin, death occurs within 10 days. The injection treatment most people have heard of only works during the incubation period; once symptoms have started, survival chances are unlikely. How The Disease Moves in the Body Virus enters an individual through broken skin and is transmitted via infected saliva. The virus invades the muscle for a few days before moving into the nearby nerves and slowly travelling to the brain. Inside the nervous system, the virus evades the immune system. The journey from nerve tissue to the brain can be slow – it is based on where the virus first enters the body. The closer the wound to the brain, the faster symptoms are seen. Once the virus moves to the brain, only days are needed before it enters salivary secretions and can be spread through bites. At this time, the infection is transmissible and symptoms begin. Stages of Noted Infection: Prodromal Stage (Days 2-3 After Symptoms Start) Personality change is evident. Friendly animals become shy, etc. The larynx begins to spasm and a voice change may be noted (especially true in rabid cattle). Most infected animals will actively lick or scratch the site of the original bite. Because of laryngeal spasms and trouble with nerves in this area, swallowing becomes difficult which is why we think of a drooling dog when we picture a visual of rabies. Excitative Stage (Day 1-7) This would be the “mad dog” stage, though, in reality, most animals skip this phase altogether. The animal has no fear and suffers from hallucinations. If confined, the animal often attacks the bars of the cage. In the prey species such as cattle, instead of aggression, a “dumbness” or stupor is noted. Paralytic Stage (Days 2-4) Weakness/paralysis sets in. The larynx is paralyzed, resulting in an inability to swallow, thus drooling and “foaming at the mouth” result. There is no treatment for animals or humans once clinical signs appear. When human exposure to the animal in question is involved, what happens depends on an assortment of criteria. If the animal in question is dead, its brain can be tested for rabies. There is no test for rabies in a living animal but since we know that death follows quickly after the virus becomes contagious, a living animal that is suspected of being rabid can be quarantined for 10 days. If the animal is still alive 10 days after biting a person and shows no neurologic changes, then the bite could not have transmitted rabies. Prevention in our pets Thankfully, rabies prevention via vaccination is readily available and very effective. There are vaccinations available for dogs, cats, ferrets and even people that work in high-risk fields (including veterinary medicine). Rabies vaccination protocols are typically controlled by local municipalities. Most communities legally require the vaccination of all dogs. The American Association of Feline Practitioners recommends rabies vaccination as a core vaccine pet cats. For pets not current on rabies vaccination that have been exposed to biting wildlife, the Texas Post-Exposure Rabies Prophylaxis Protocol has been particularly helpful. Here, the pet should be vaccinated for rabies as soon as possible after the wildlife bite with booster vaccines given three weeks post-bite and eight weeks post-bite. The pet should be strictly isolated for 90 days. This protocol has been extremely successful in preventing rabies symptoms and contagion when normal rabies vaccination had lapsed. For people – if you are bitten by an animal (even a domestic dog or cat) and its rabies vaccination history is unknown, there are steps to take. A fresh bite wound should be washed out with water quickly as this may wash out viral particles. The time it takes for the virus to reach the brain depends on how close the wound is to the brain. This simple step can be life-saving. If the biting animal is alive, its vaccination status should be confirmed as soon as possible and it will need to be confined according to local law. The bite wound should be reported to the health department as soon as possible. Please note, rodent and rabbit bites are not reportable. If the animal is dead then its brain can be tested for rabies. The head of the biting animal is submitted to the health department for special testing. This process takes a matter of hours so that any bite victims can know right away if they will require rabies treatment. If the animal is not available or its vaccination status is in question, further treatment may be needed. humans should consult their human medical doctor immediately for protocols and possible preventative treatment.
Runny Diarrhea in Dogs and Cats

What is Colitis – the cause of mucoid gooey stool? Colitis means that the colon or large intestine is inflamed. The hallmark of colitis is a gooey, frequent diarrhea that may contain blood and/or mucus. The stool may start normal then finish soft or may seem gooey throughout. There is often accompanying gas and the sudden need to run for a bathroom. Vomiting can go along with colitis but the primary feature is the gooey diarrhea. Colitis may happen suddenly or can be going on for a while. Weight loss is often not a common feature. A Little About the Colon the colon/lower intestine is the last segment of the digestive tract. Before reaching the colon, food has been digested and mostly absorbed. What’s left is the waste products from food, the feces, and this is eliminated by the colon. The colon has three functions: The bacterial population in the colon is about 10 times more dense than that of the small intestine. These bacteria, often referred to as good or helpful bacteria, take fibers that were undigestible to the host and actually process them into biochemicals that provide nourishment to the colon cells. The bacteria that live in the colon not only feed the cells of the colon, but they also control the pH of the colon environment so that excreted toxins are trapped in the stool and will be pooped away rather than be reabsorbed back into the body. Diarrhea Can Come from Either the Small Intestine or the Large Intestine and the Approach is Different in Either Case In classifying diarrhea, it is important to determine whether the problem originates from the small intestine, the colon, or possibly both. Small intestinal diarrheas tend to be more serious as it involves problems digesting and absorbing nutrients from food. Diarrhea of the colon is less debilitating but still uncomfortable. The following are characteristics of large intestinal diarrhea: A diagnosis of colitis is generally straight forward given the above classic findings, though how to proceed depends on the signs. Is the problem acute (i.e., suddenly there) or chronic (has been happening for several weeks regularly) or episodic (happens then goes away then happens again)? Colitis Suddenly A pet that has sudden symptoms of colitis probably has a stress-related colitis (common after boarding, moving, severe weather or other change) or a dietary indiscretion-related colitis (usually involves treats or raiding the garbage). These episodes should be treated immediately as they can get worse if left untreated. That said, in general, colitis can be treated with a short course of medication such as metronidazole, probiotics and dietary therapy. Parasites, especially Giardia and whipworms, can also cause colitis and the pet may be tested for those to rule them out or be dewormed. In general, a few days of medication and a bland diet should resolve the problem and the pet will be back to normal quickly. During recovery, it is common for the pet to have no stool at all for a couple of days. This is normal and not a sign of constipation. If, however, the pet’s diarrhea is not clearly improved in two to three days, contact the veterinarian to see if further testing is needed. Colitis Chronically or in Recurrent Episodes If the symptoms of colitis have been going on for a month or more or if they keep recurring and resolving over and over, then a medical work up is needed. It is important to make sure simple causes of colitis have been ruled out, so parasite testing becomes especially important. A good fecal examination for worms and coccidia plus testing additional for giardia should be performed. If any of these tests are positive, then obviously the parasite in question can be addressed; it is always best to identify the cause of the colitis if it is possible to do so. That said, even if these tests are negative, it is still a good idea to include a broad spectrum de-worming and coccidia treatment should probably be given as these treatments are safe and inexpensive. Whipworms, in particular, are difficult to detect and commonly cause colitis symptoms. We want to be sure we have ruled out the simple causes of colitis before more advanced diagnostics begin. Similarly, a week or so of metronidazole may effectively treat a toxin-producing Clostridium perfringens infection and potentially solve the entire problem. Of course, a basic blood panel and urinalysis are in order, as they are with any chronic disease, to assess the patient’s general health. If all the regular diagnostics are negative or inconclusive, there is a fecal panel that amplifies DNA of bacterial and protozoal organisms that cause diarrhea. Talk to your veterinarian about this. Further workup can be initiation of a hypoallergenic diet for food allergies/sensitivities as well as inflammatory bowel disease (IBD). To make a definitive diagnosis of IBD, colonoscopy and intestinal biopsies Management of Colitis Colitis is best managed when its cause is known and specific therapy can be instituted. When this is not possible, symptomatic management as described above is often attempted. Boxers and Some Other Breeds Can Get a Specific Form of Colitis This condition is also called Boxer colitis because the Boxer breed seems predisposed. This form of colitis is particularly ulcerative and involves infiltration of the tender colon lining with cells called histiocytes. These cells are the cells that are normally called into the scene of inflammation relatively late so that they can absorb the dead cells and debris that have been created by the inflammatory event. Dogs with this condition typically show symptoms at an early age (less than two years) and become more debilitated than typical colitis patients. It is currently believed that this condition results from an inappropriate immune response against the common bacteria of the colon, especially E. coli. Dogs with this form of colitis do not respond well to the usual remedies listed above but instead seem to show an excellent response to one class of antibiotic. Histiocytic ulcerative colitis can be confirmed by biopsy, although signs of colitis in a young Boxer
Pet Treats…The Do and Dont’s

Pet treats are widely used, and for good reason. Treats can be useful training tools, and pets typically like treats (and owners like to make their pets happy). But even something as simple as feeding pets treats carries some risks. Finding the right treat is essential. Many pet owners don’t realize that some common treats have bacteria and other things that can make your pet sick! Pathogens Toxins The main concern here is chicken, duck and sweet potato jerky treats from China, which have been implicated in a large number of pet illnesses and deaths, including at least 1000 dead dogs. No main factor has been found that cause the kidney issues associated with these treats, so there’s no way to test the products to ensure the same problem won’t happen again. Injuries Obstructions Dogs eat stuff they’re not supposed to all the time (at least mine does). Most often, it’s not a problem, but sometimes it is. If a pet swallows a large piece of a poorly digestible treat it can cause an issue in the esophagus if it’s too large and gets stuck. Realistically, this is of limited concern for most edible treats, but is a bigger issue with toys and things like rawhides. If using rawhide treats, make sure to get an appropriate sized one for your dog. While enjoying treats such as rawhide, pets should be supervised Obesity A tasty and cherished cat treat is pictured below – It comes in variety flavor packs and single flavor packs. The cats we polled seemed quite keen on the Tuna flavor. Weight gain and obesity aren’t usually considered when thinking about problems with treats, but a lot of treats are high in calories, and obesity isn’t just a problem with pet owners. As with human snacking, moderation is the key. Before giving it to your pet, think about the treat, how to use it and what problems might occur. Most treats, particularly those that are not raw animal product based (e.g. pig ears), not prone to fragmenting (e.g. bones, especially cooked bones) and not excessively hard (e.g. bones) are fine in moderation. If you’re unsure about the safety of a treat or chew toy, please reach out to your family veterinarian for suggestions.
Testicular Tumors in Dogs

Testicular tumors are the most common genital tumors found in male dogs. Tumors can grow in one or both testicles. Most types of testicular tumors are malignant. Usually this means that they are cancerous and have the potential to spread and harmfully change the surrounding tissues. Cancerous tumors can also metastasize (spread) to other organs throughout the body. But, the good news is that although testicular cancer in dogs is technically malignant, unlike other types of malignant tumors, these tend to occur at an older age (i.e. average 10 years of age) and metastasis to other organs is rare. Caught early, castration, even at an older age, is usually curative. Dogs have three main types of testicular cancer (although numerous uncommon cancers can occur): More than one of these three types can occur in one cancerous testicle, and both testicles can be cancerous but have different types of testicular cancer. Symptoms When a dog has testicular cancer ( a tumor), one of his testicles may look or feel abnormal. The affected one may be larger or it may have a firm and lobulated feel, some are painful. In crytporchid intact males (dogs that have only one descended testicle) cancer of the undescended or cryptorchid testicle is common but will not be obvious by just looking at your pet since it is inside your dog’s body. Sertoli cell tumors and seminomas are the most common types of testicular cancer found in an undescended testicle. Other symptoms of cancer can include weight loss, poor appetite, abdominal/belly pain, or a mass in the belly. Some testicular cancers, such as the Sertoli cell tumors, produce estrogen, a hormone more commonly associated with female dogs. If there is such a tumor, you may also see enlarged mammary glands or breast tissue; hair loss on the dog’s trunk; or dark discoloration to the skin. Leydig cell tumors can produce an excess amount of testosterone. In this case, you may notice your dog has swelling on his rear near his anus, which may be due to a hernia or enlargement of the perianal glands surrounding the anus. In severe forms of testicular cancer that are more aggressive or malignant, the bone marrow can be affected. This can result in anemia or decreased red blood cells in the blood stream; low platelets and bruising; or abnormalities with white blood cells. It is important to understand that initially many dogs will not show obvious symptoms. What to do if you Suspect Testicular Cancer If you think your dog might have testicular cancer, your regular veterinarian will perform a physical examination of your dog’s testicles. A rectal examination will check your dog’s prostate gland and feel for enlarged lymph nodes. Palpation or feeling structures inside your dog’s abdomen is also common, as well as checking your the gums and listening to the heart and lungs. If cancer is suspected, x-rays of the belly and chest may be needed to search for more clues of cancer or spread to other organs. Lab work may be done to make sure your pet’s internal organs are functioning correctly or to see what hormones are circulating in the bloodstream. Sometimes an abdominal ultrasound will be needed to look for metastasis. Again, the majority of these tumors if addressed early on, will not spread to other organs. Treating Testicular Cancer Castration, or basic neutering, is the recommended treatment of choice. Both testicles need to be removed because cancer may be in both even if only one is obviously affected. If a pet is cryptorchid, intra-abdominal surgery will be needed to remove the testicle in the abdomen as well as surgery to remove the normal one. A pathologist can assess the testicles after they are removed to determine the type of cancer. Sometimes chemotherapy or radiation can be performed, but the effectiveness will depend on the type and severity of cancer. If your veterinarian is not comfortable treating the type of cancer, you may be referred to a veterinary oncologist. If no evidence of metastasis has occurred, surgery is often the only treatment needed and your pet will be cured. Pets that are severely affected by testicular tumors, such as those with bone marrow disease or spread to other organs have a poorer prognosis. This means that even with surgery, very sick pets may not survive. The sooner surgery can be performed after noticing symptoms or a change in the testicles, the better your pet’s chances of cure will be. Prevention Neutering your pet before he develops cancer will prevent testicular cancer. This is especially important if your pet is cryptorchid as testicular cancer is more common in an undescended testicle.
How To Care for Orphan Puppies & Kittens

At some point or another, we usually find baby animals that we wish we hadn’t seen. Kittens or puppies that are too small to care for themselves and without a mother in sight or an injured or dead mother. In other instances a bitch or queen produces a little but proves that they are unable to care for their young. In these instances, we need to care for the puppies or kittens until they are old enough to eat on their own and be placed in responsible homes. Below are the things you can do to help orphaned young thrive: The Nest Box Keep the babies together as long as they are about the same age; this will help socialize them to their own species and will help in keeping them warm. Try to assemble the following equipment. If a neonatal puppy or kitten’s temperature drops below 94⁰F, the heart rate drops and intestinal motion ceases. Death will occur if this is not fixed. If this happens, slowly warm the babies over 1-2 hours so they can slowly be warmed up to an appropriate body temperature The Diet Makeshift Formula Until Commercial Formula can be Obtained Puppies 1 cup whole milk1 tsp. salad oil1 drop multi-vitamins (if you have any)2 egg yolks Kittens1/2 cup whole milk1 egg yolk1 drop multi-vitamins3 crushed Tums (antacid) For either one, then mix in a blender. The Bottle How / When To Feed Urination / Defecation Expect the baby to need stimulation for urination/defecation for the first three weeks of life. Bathing Keeping On Track Starting Solid Food The best way to be sure everything is going well is to track weight gain in your new babies. A postal scale or food scale (ideally one that measures weight in grams) will be helpful. A puppy or kitten should gain 10% of the birth weight every day and should be drinking 22 to 26 cc of formula per 100 grams of body weight over the course of the day. Puppies are variable in growth expectancy depending on breed, but kittens are more predictable and should gain 50 to 100 grams weekly. Kittens weighing less than 90 grams (approx three ounces) at birth have a high (59%) mortality rate. A Note on Colostrum Colostrum is the first milk produced by the mother shortly after giving birth. It is rich in antibodies which will protect the babies for the first several months of life. Colostrum is only produced for a day or two and the baby is only able to absorb its antibodies for a day or two. Without colostrum (if their mother did not nurse the kittens during the first two days of life) the babies are left with serious immunological disadvantages. Especially great care should be taken in cleanliness and the babies can be vaccinated as early as age two weeks depending on circumstances. They may require a plasma transfusion to make up for the colostrum. There is no substitute for a real mother. Many foster parents have difficulty distinguishing male and female kittens at this early age. See your veterinarian to help you in determining the kitten’s sex.
Not Eating (or Anorexia) in Dogs and Cats

Appetite loss and reduction are important factors in many diseases and they must be recognized and addressed as quickly as possible. Nutrition and lack of nutrition is essential in preventing further issues. Acceptance of favorite foods often determines if a pet should be hospitalized or not. A couple of off days is generally not a big problem as long as the pet maintains hydration by his or herself or is given fluids by your family veterinarian. But ongoing issues of poor or no appetite can make matters worse and also suggest a primary ongoing health issue. Nutritional support not only helps the pet recover but buys time to keep the pet stable while diagnosis and treatment are worked out. The pet must be eat and drink in order to get well. The term anorexia simply means eating no food. When the veterinarian says the pet has anorexia, it does not mean the pet has a distorted body image; it means the pet is not eating. So how do we get a pet to eat? We will review some techniques here. Be sure to check with your veterinarian regarding the proper amount of food to feed and which foods are acceptable. Pets with poor appetite are sick, and if you wait until the appetite is completely gone it may make recovery harder. This is particularly true for cats. As the appetite fades, the pet must depend on stored fat for nutrients. When large amounts of fats are mobilized to meet energy demands, they must be processed by the liver before being used for calories. Cats are prone to developing a disorder called fatty liver disease or hepatic lipidosis. First Offer Canned Food If you think your pet’s appetite is poor but are offering only kibbled food, your first step is to get some smelly canned food and offer that. Most animals find canned diets far more tasty than dry foods and you may find that this step alone fully alleviates the problem. There is a misconception that canned food is somehow of poor nutritional quality. In fact, canned food and dry food are different mostly with regards to water content. Canned foods are about 70% water differ primarily in their water content and thus in texture. If you consider the food without water, the unprepared diet is basically a powdered meat mix similar to a flour. See if the pet will eat a canned food or mixture of dry and canned food. Additionally, one can add a flavored broth or cooked egg to try and encourage your pet to eat a kibbled diet. Second, Offer a Delicacy Foods that are generally regarded as delicacies among pets include: canned chicken, cooked egg, and canned tuna. With the exception of the recovery diets, treats are not nutritionally complete but can make a good jump starter for pets to get them eating over the first few days or a week. Long-term use as the sole food is not recommended. A pet who has not been eating may feel continued discomfort until eating begins again. Something tasty may be necessary to get the appetite re-started. To get your pet interested, rub a small amount on the teeth or spoon a little in the mouth so that the pet can get a taste. Don’t be surprised if he spits it out; we are just trying to get the taste of the food in his / her mouth. Hold the bowl up to the pet’s nose so that the aroma is inescapable. You may find that coaxing in this way gets the appetite started. A Note on Gourmet Cat Foods (Yes, Dogs Eat Them, too) Several “extra tasty” products available in the grocery store can be really helpful in tempting a pet with a poor appetite. Fancy Feast by Purina comes in numerous textures and flavors, each can containing approximately 100 calories. The diet is complete and balanced for cats and is often a good appetite jump starter. Temptations, by Mars Pet care, are especially well accepted treats made for cats. Because many cats will not eat anything else, they have been balanced to be nutritionally complete for cats and can be used as a cat’s sole diet if necessary. A Note on Starting Prescription Diets If the pet is supposed to eat a prescription diet but refuses, do not attempt to starve the pet into eating the prescription food. Many prescription diets are relatively bland and pets do not wish to eat them, particularly if they are used to eating large amounts of table scraps (always a bad practice) or a more flavorful regular food. Starving the pet will only make him sicker. Try a gradual change from the regular food to the new food over a week or so. If the pet simply will not accept the new food, be sure to let your veterinarian know this. There may be an alternative flavor to try; further, prescription diets are guaranteed by the manufacturer meaning you can get a full refund on the bag or case if the pet does not accept the food. Sometimes it is necessary to forgo the therapeutic aspect of the special diet just to get the pet to eat but your veterinarian will help you with these guidelines. Provide Privacy Be sure other pets at home do not bully or distract the sick pet. In a multi-pet home, it may be difficult for the sickly or elderly pet to eat without the younger pets taking his food. Many animals wish to eat at their leisure, particularly if they do not feel well. Consider giving your pet a private area and her own dish. Never feed multiple pets from the same bowl as one is sure to get the lion’s share of the food to the other’s disadvantage. Many pets like to eat overnight when no one is watching. Medical Assistance Appetite-stimulating medications are available. There are several products available that can create a sense of hunger. Capromorelin (brand name Entyce): This is a
Heart Murmurs in Dogs and Cats
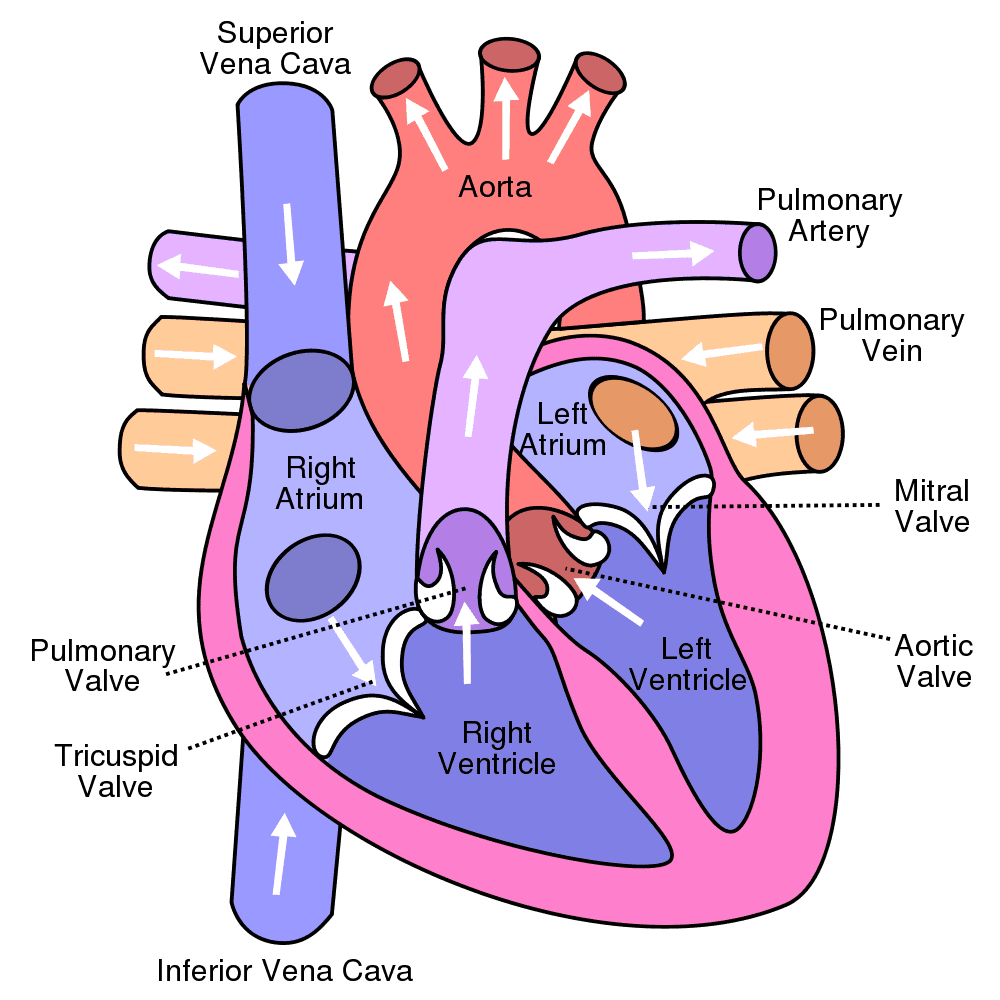
What does a murmur mean? A heart murmur is an abnormal sound your veterinarian can hear when listening to your pet’s heart with a stethoscope. Normally, two distinct sounds are heard when listening to the heart of a normal dog or cat. These are often described as “lub” and “dub.” When listening with a stethoscope one typically hears a: Lub-dub…Lub-dub… sound. A murmur is an abnormal sound that often sounds like a whoosh in between the lub and the dub. extra sound, which can sometimes drown out the normal sounds. What causes a heart murmur? The short answer is turbulent blood flow. Like the water in a calm river or stream, normally blood flows through the heart in a quiet, smooth manner. But, if something obstructs the flow, turbulence is created. The same happens with blood flow through the heart. Lots of things can cause turbulent flow. To understand what can, have a look at the heart anatomy above. If any of the valves is too small or to large, normal blood flow changes. Some of these changes occur with aging. In a younger animal, a murmur heard may represent a birth defect and be congenital. The most common murmurs in older dogs are associated with leaky mitral valves. In young cats, thickening of the ventricle walls called hypertrophic cardiomyopathy is a congenital issue. So, there are many reasons from valvular issues, to constriction of valve size to defects between chambers. Finally, turbulence can be heard when the blood is too thin (anemia) or even when a patient is very excited, causing the heart to pump faster and harder than normal. Are different types of murmurs associated with specific diseases or conditions? the short answer is yes, but it’s a little more complex. Murmurs are caused by different structures inside and outside the heart. Your veterinarian can use various clues about the murmur to try to determine what the likely origin is. For instance: murmurs associated with patent ductus arteriosus are continuous when auscultated in the left armpit while murmurs associated with ventricular septal defects tend to be loudest on the right side (as are murmurs associated with leaky tricuspid valves). That said, sometimes, it’s impossible to tell the exact nature. Often chest x-rays and a cardiac ultrasound 9echocardiogram) will be recommended. This is especially the case in cats, where most murmurs are heard near the sternum. What is a benign or “innocent” murmur? Some heart murmurs are called benign (or innocent or physiological), meaning there is no apparent heart disease that explains the murmur. These murmurs are often seen in puppies and can occur in cats of any age. They are uncommon in adult dogs. Benign murmurs are usually soft (rather than loud) and can be intermittent. Benign puppy murmurs will generally disappear by 12 to 15 weeks of age. My pet’s murmur has a grade. What does this mean? Murmur grading is simply your veterinarian’s way of describing the loudness of a murmur. Most veterinarians grade murmurs on a scale from 1 to 6. The lower the grade, the quieter the murmur. However, it is often easiest to simply describe them as “soft,” “moderately,” “loud” or “palpable” (where you can feel the murmur like a vibration through the chest). The grade or loudness of the murmur is only sometimes related to the severity of the heart abnormality causing it. Remember, grading a murmur is subjective because it is based on how it sounds to the listener. Also, it’s hard to tell if an animal has a heart murmur if the pet is excited or anxious because rapid breathing sounds can mimic a murmur. As a general rule, if a murmur is heard in a patient older than 4 months, it is a good idea to work with your veterinarian and obtain diagnostics such as chest x-rays and an echocardiogram so the origin and severity of the issue can be determined and, if needed, addressed.